| Weight : | birth 2, 4, 6, 8, 12, 16 weeks, 6-8 months, 1 year. |
| Length : | 10 days and 3 monthly up to year 1. |
| Height : | Yearly from 18 months, school entry and routine checks at school. |
| Head Circumference : | 36 hours, 10 days and 8 weeks and as indicated. |
If there is any concern about growth, measurements should be taken more frequently.
| Is this child small/tall but appropriate for parental heights? | Yes | Normal short/tall stature |
| Is child inappropriately short/tall for parental heights? | Yes | Refer to Paed Endocrinologist |
| Is child growing at an inappropriate growth rate? |
| Small for chronological age | GROWTH DELAY |
| Abnormal karyo type | CHROMOSOME ABNORMALITIES • Turner Syndrome • Down’s Syndrome |
| Low brithweight, thin, dysmorphic, possible asymmetry | INTRAUTERINE GROWTH RETARDATION (IUGR) • Including Russel Silver syndrome |
| Dysmorphic, cardiac problems | NOONAN SYNDROME |
| Abnormal hypopituitary function | ENDOCRINE DISORDERS • Growth hormone insufficiency • Panhypopituitarism • Hypothyroidism • Cushing's Syndrome • Premature sexual Maturation • Environmental growth failure |
| Dysmorphic | BONE DYSPLASIAS • Achondroplasia • Hypochondroplasia |
| Chronic ill health | CHRONIC DISEASES • Congenital heart disease • Renal failure • Coeliac/Crohn’s disease • Cystic Fibrosis • Asthma / eczema |
| Inappropriate tall stature | SYNDROMES • Marfan • Sotos • Klinefelter’s ENDOCRINE • Precocious puberty |
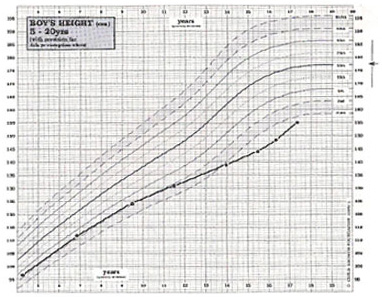 All children who are considered short/tall should be assessed for their MPC and TCR (see page 5). If their height is within normal limits for their parents and they are growing at a normal rate, they are normal, whatever their position within the population standards.
All children who are considered short/tall should be assessed for their MPC and TCR (see page 5). If their height is within normal limits for their parents and they are growing at a normal rate, they are normal, whatever their position within the population standards.
There is no effective treatment for genetic short stature. The availability of biosynthetic growth hormone has allowed increased interest in the use of this substance for the treatment of children who are very short. This is still in the stage of clinical trials but available evidence suggests that final stature will not be altered significantly. While it is clear that even in children with normal growth hormone secretion, a short-term acceleration in growth may be achieved during growth hormone therapy, there is no certainty at this time that the long-term final height prognosis is altered. Further careful studies, extending over a number of years, will be necessary to show this. However, in the USA, there is a much more liberal treatment regimen for children with genetic short stature. Although this probably represents a very heterogeneous group of children, growth hormone is now licensed for use in this indication.
Constitutional delay of growth in puberty (CGDP) frequently causes concern and seems to be more prevalent in boys than girls. It is often first noticed when the boy seems to have stopped growing, has younger siblings catching up or even being taller than him, or has classmates leaving hi behind. Growth delay of up to two years is not uncommon and a small number of children are delayed three, or even four years. Frequently one of the parents, an aunt or an uncle, brother or sister, will have had growth delay. A mother will often be able to establish that she was 15 or more years old at menarche instead of the more usual 12 to 14 years : it may be more difficult to establish a father’s pubertal delay owing to the lack of a fixed event such as menarche.
Once growth delay has been established any boy or girl can be absolutely reassured that puberty occurs in the end and that they will develop quite normally in every way. They can be reassured with a full demonstration of facts, figures, charts and predictions. Children find the information that they are simply taking after their mothers or fathers reassuring if not particularly welcome. What reassurance does not do is remove the very real physical handicap associated with being small and, worse, remaining pre-pubertal with a peer group of adolescents.
For Appointment :